If elevated low density lipoprotein cholesterol (LDL-C) levels were the only source of cholesterol deposited in the artery wall, then high doses of potent statins should be reversing (rather than reducing) the build-up of atherosclerotic plaques, largely eliminating deaths from coronary heart disease (CAD). Sadly, the number one cause of death in Americans taking statins to lower their elevated LDL-C to prevent heart attacks is still heart attacks?
If elevated low density lipoprotein cholesterol (LDL-C) levels were the only source of cholesterol deposited in the artery wall, then high doses of potent statins should be reversing (rather than reducing) the build-up of atherosclerotic plaques, largely eliminating deaths from coronary heart disease (CAD). Sadly, the number one cause of death in Americans taking statins to lower their elevated LDL-C to prevent heart attacks is still heart attacks?
Yes, statin drugs are very effective for reducing high LDL-C levels, and they do slow the progression of cholesterol-filled plaques. However, they rarely reverse the build-up of cholesterol in the artery wall. More importantly, statin drugs alone do not come close to eliminating the risk of heart attacks and most strokes despite impressive reductions in LDL-C levels. Research now shows that other lipoproteins besides LDL particles can and do carry cholesterol from the blood into the artery wall, promoting the growth of cholesterol-filled plaques and CAD. These lipoproteins are neither LDL-C or high density lipoprotein cholesterol (HDL-C), but rather consist of the cholesterol-rich remnants of triglyceride-rich lipoproteins produced by the liver (VLDL) and the small intestine (chylomicrons)(1). Both genetic factors and dietary factors influence the amount of these triglyceride-rich lipoproteins produced and also the amount of cholesterol-rich remnant particles derived from each of them in the blood. Fat and cholesterol-rich meals can dramatically increase the production of chylomicrons and lead to greater amounts of cholesterol-rich chlyomicron remnants in the blood for several hours after each fat-rich meal (2).
Dr. Borge Nordestgaard’s recent study followed nearly 12,000 people with established CAD in Denmark and found that each 1 mmol (38.7 mg/dl) increase in non-fasting remnant cholesterol caused 2.8 times greater risk of a CAD event that was independent of HDL-C levels. The increased causal risk of CAD from elevated cholesterol remnant particles appeared much stronger than for changes in either LDL-C or HDL-C levels (3). Most doctors (MDs) now check only fasting blood lipids and focus largely on LDL-C and HDL-C to assess their patient’s future CAD risk. This was based on the simplistic notion that it was only the LDL-C particles delivering cholesterol to the artery wall, making it the “bad” cholesterol, while the HDL-C particles were removing the cholesterol from the artery wall and bringing it back to the liver, making their cholesterol content “good”. Of course, we now know HDL-C particles can actually become proinflammatory and proatherogenic “bad” HDL particles, perhaps partly in response to biochemical changes in the HDL particles triggered in part by chylomicrons and other remnant cholesterol particles in the blood.
Chylomicrons and their cholesterol-rich remnants remain in the blood for several hours after each fat-rich meal and likely play a major role in promoting inflammation (by increasing IL-6 & CRP), thrombosis (by activating clotting factor VII), and atherosclerosis (by delivering more cholesterol-rich remnant particles to the artery wall). The fact that damage to the endothelium (inside “skin” of the artery wall) as evidenced by reduced flow mediated dilation (FMD) occurs to a much greater extent after a single fat-rich meal than after a meal high in carbohydrate points to the fact that pathological changes must be occurring in the artery wall in response to fat and cholesterol-rich particles coming from the intestines (4). Indeed, this reduced FMD is likely the main reason why many people with angina tend to experience far more chest pain after a large, fat-rich meal than they do after a meal high in carbohydrate-rich plant foods. The only legitimate debate is not whether LDL-C or other cholesterol-rich remnant particles promote atherosclerosis and increase the risk of CAD, but rather which is more atherogenic. Clearly both LDL-C and other remnant lipoprotein particles deliver cholesterol to the artery wall and promote foam cell formation and atherosclerosis. Unlike LDL-C particles (which must first be oxidized), remnant cholesterol particles are readily taken up by scavenger receptors of macrophages in the cell wall to form foam cells (5,6). Increasing evidence suggests that damage to the artery wall from cholesterol-rich remnant particles appears to be at least as important as either fasting LDL-C or HDL-C levels for predicting future CAD events.
It should be noted that diets high in refined carbohydrates (particularly large amounts of refined sugars) combined with inactivity can contribute to a marked increase in the liver’s production of VLDL particles because the liver converts some of the excess carbohydrate (especially fructose) into triglyceride. This leads to more triglyceride-rich VLDL particles being released into the blood, which then degrade into cholesterol-rich remnant particles and eventually also LDL particles. This is particularly true in people who are genetically prone to develop insulin resistance and type 2 diabetes and who experience significant increases in fasting triglyceride levels as visceral fat stores accumulate.
Bottom Line: Reducing LDL-C levels with statin drugs alone is insufficient for stopping and reversing CAD and preventing most heart attacks and strokes. A diet low in fat, salt, cholesterol, and refined carbohydrates coupled with increased activity and loss of excess weight may also be necessary to stop and reverse CAD in part by reducing remnant cholesterol levels in the blood.
By James J. Kenney, PhD, FACN
Sources:
- Mark Nordestgradd BG, Freiberg JJ. Clinical relevance of nonfasting and postprandial hypertriglyceride and remnant cholesterol. Curr Vasc Pharm. 2011;9:281-6
- Mark Cesar TB, et al. High cholesterol intake modifies chylomicron metabolism in normolipidemic young men. J Nutr 2006;136:971-6
- Mark Varbo A, et al. Remnant cholesterol as a causal risk factor for ischemic heart disease. J Am Col Cardiol. 2013;61:427-36
- Mark Tomaino RM, Decker EA. High-fat meals and endothelial function. Nutr Rev. 1998;56:182-5
- Mark Zilversmit DB. A proposal linking atherogenesis to the interaction of endothelial lipoprotein and triglyceride-rich lipoproteins. Circ Res.1973;33:633-8
- Mark Nakajima K, Nakano T, Tnaka A. The oxidative modification hypotheis of atherosclerosis: the comparison of atherogenic effects of oxidized LDL and remnant lipoproteins in plasma. Clin Chim Acta. 2006;367:534-42
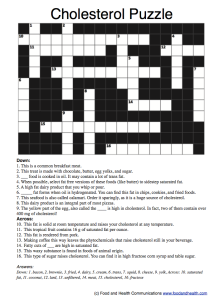
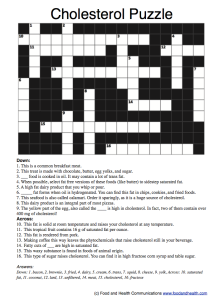
Looking for fun ways to improve your clients’ understanding of cholesterol and its health risks? Check out this free handout: Cholesterol Puzzle.
And, as you well know, there are tons of other heart health education materials available in the Nutrition Education Store. Pay special attention to the posters, which have been flying off the shelves lately!

LDL Cholesterol Poster
Premium Heart Health Education Kit
Heart Health Brochure: Lower Your Heart Attack Risk
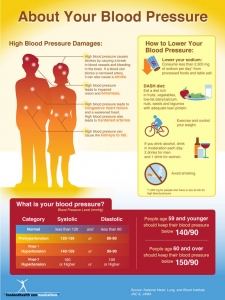
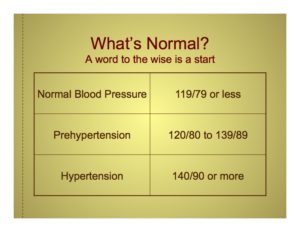
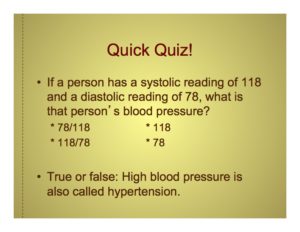
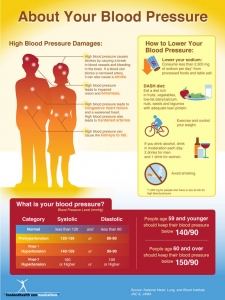
Blood Pressure Poster